- Confirm the diagnosis and classify diabetes. A
- Evaluate for diabetes complications, potential comorbid conditions, and overall health status. A
- Review previous treatment and risk factor management in people with established diabetes. A
- Begin engagement with the person with diabetes in the formulation of a care management plan including initial goals of care. A
- Develop a plan for continuing care. A
SARS-CoV-2 Vaccines and Other Immunizations
The importance of routine vaccinations for people with diabetes has been elevated by the coronavirus disease 2019 (COVID-19) pandemic. Preventing avoidable infections not only directly prevents morbidity, but also reduces hospitalizations, which may additionally reduce the risk of acquiring infections such as COVID-19. Children and adults with diabetes should receive vaccinations according to age-appropriate recommendations.
In people with diabetes, higher blood glucose levels prior to and during COVID-19 admission have been associated with poor outcomes, including mortality. People with diabetes should be prioritized and offered SARS-CoV-2 vaccines.
Assessment of Selected Comorbidities
Cancer
People with diabetes should be encouraged to undergo recommended age- and sex-appropriate cancer screenings and to reduce their modifiable cancer risk factors (obesity, physical inactivity, and smoking).
Cognitive Impairment/Dementia
See “13. OLDER ADULTS.”
Nonalcoholic Fatty Liver Disease
Recommendation
- 4.10 People with type 2 diabetes or prediabetes with cardiometabolic risk factors, who have either elevated liver enzymes (ALT) or fatty liver on imaging or ultrasound, should be evaluated for presence of nonalcoholic steatohepatitis and liver fibrosis. C
5. Facilitating Positive Health Behaviors and Well-Being to Improve Health Outcomes
Essential to achieving diabetes treatment goals are DSMES, medical nutrition therapy (MNT), routine physical activity, tobacco cessation counseling when needed, health behavior counseling, and psychosocial care.
DSMES
Recommendations
- 5.2 There are four critical times to evaluate the need for DSMES to promote skills acquisition to aid treatment plan implementation, MNT, and well-being: at diagnosis, annually and/or when not meeting treatment targets, when complicating factors develop (medical, physical, psychosocial), and when transitions in life and care occur. E
- 5.4 DSMES should be person-centered, may be offered in group or individual settings, and should be communicated with the entire diabetes care team. A
- 5.5 Digital coaching and digital self-management interventions can be effective methods to deliver DSMES. B
- 5.9 Consider addressing barriers to DSMES access through telehealth delivery of care B and other digital health solutions. C
MNT
All HCPs should refer people with diabetes for individualized MNT provided by a registered dietitian nutritionist who is knowledgeable and skilled in providing diabetes-specific MNT.
Goals of Nutrition Therapy for Adults With Diabetes
- To promote and support healthful eating patterns, emphasizing a variety of nutrient-dense foods in appropriate portion sizes, to improve overall health and:
- Achieve and maintain body weight goals
- Attain individualized glycemic, blood pressure (BP), and lipid goals
- Delay or prevent diabetes complications
Assessing Food Insecurity
Any member of the health care team can screen for food insecurity using The Hunger Vital Sign. Households are considered at risk if they answer either or both of the following statements as “often true” or “sometimes true” (compared with “never true”):
“Within the past 12 months, we worried whether our food would run out before we got money to buy more.”
“Within the past 12 months, the food we bought just didn’t last, and we didn’t have money to get more.”
Physical Activity
Recommendations
- 5.28 Children and adolescents with type 1 diabetes C or type 2 diabetes or prediabetes B should engage in 60 minutes/day or more of moderate- or vigorous-intensity aerobic activity, with vigorous muscle-strengthening and bone-strengthening activities at least 3 days/week.
- 5.29 Most adults with type 1 diabetes C and type 2 diabetes B should engage in 150 minutes or more of moderate- to vigorous-intensity aerobic activity per week, spread over at least 3 days/week, with no more than 2 consecutive days without activity. Shorter durations (minimum 75 minutes/week) of vigorous-intensity or interval training may be sufficient for younger and more physically fit individuals.
- 5.30 Adults with type 1 diabetes C and type 2 diabetes B should engage in 2–3 sessions/week of resistance exercise on nonconsecutive days.
- 5.31 All adults, and particularly those with type 2 diabetes, should decrease the amount of time spent in daily sedentary behavior. B Prolonged sitting should be interrupted every 30 minutes for blood glucose benefits. C
- 5.32 Flexibility training and balance training are recommended 2–3 times/week for older adults with diabetes. Yoga and tai chi may be included based on individual preferences to increase flexibility, muscular strength, and balance. C
- 5.33 Evaluate baseline physical activity and sedentary time. Promote increase in nonsedentary activities above baseline for sedentary individuals with type 1 diabetes E and type 2 diabetes. B Examples include walking, yoga, housework, gardening, swimming, and dancing.
Smoking Cessation: Tobacco and E-Cigarettes
Recommendations
- 5.34 Advise all individuals not to use cigarettes and other tobacco products or e-cigarettes. A
- 5.35 After identification of tobacco or e-cigarette use, include smoking cessation counseling and other forms of treatment as a routine component of diabetes care. A
Psychosocial Care
Recommendations
- 5.38 Psychosocial care should be provided to all people with diabetes, with the goal of optimizing health-related QoL and health outcomes. Such care should be integrated with routine medical care and delivered by trained HCPs using a collaborative, person-centered, culturally informed approach. A When indicated and available, qualified mental health professionals should provide additional targeted mental health care. B
- 5.39 Diabetes care teams should implement psychosocial screening protocols that may include but are not limited to attitudes about diabetes, expectations for treatment and outcomes, general and diabetes-related mood, stress and/or QoL, available resources (financial, social, family, and emotional), and/or psychiatric history. Screening should occur at periodic intervals and when there is a change in disease, treatment, or life circumstances. C
- 5.40 When indicated, refer to mental health professionals or other trained HCPs for further assessment and treatment for symptoms of diabetes distress, depression, suicidality, anxiety, treatment-related fear of hypoglycemia, disordered eating, and/or cognitive capacities. Such specialized psychosocial care should use age-appropriate standardized and validated tools and treatment approaches. B
- 5.42 Routinely monitor people with diabetes, caregivers, and family members for diabetes distress, particularly when treatment targets are not met and/or at the onset of diabetes complications. Refer to a qualified mental health professional or other trained HCP for further assessment and treatment if indicated. B
Sleep Health
Recommendation
- 5.55 Consider screening for sleep health in people with diabetes, including symptoms of sleep disorders, disruptions to sleep due to diabetes symptoms or management needs, and worries about sleep. Refer to sleep medicine and/or a qualified behavioral health professional as indicated. B
6. Glycemic Targets
Assessment of Glycemic Control
Glycemic control is assessed by the A1C measurement, continuous glucose monitoring (CGM) using time in range (TIR) and/or glucose management indicator (GMI), and blood glucose monitoring (BGM).
Glycemic Assessment
Recommendations
- 6.1 Assess glycemic status (A1C or other glycemic measurement such as TIR or GMI) at least two times a year in patients who are meeting treatment goals (and who have stable glycemic control). E
- 6.2 Assess glycemic status at least quarterly and as needed in patients whose therapy has recently changed and/or who are not meeting glycemic goals. E
Glucose Assessment by CGM
Recommendations
- 6.3 Standardized, single-page glucose reports from CGM devices with visual cues, such as the ambulatory glucose profile (AGP), should be considered as a standard summary for all CGM devices. E
- 6.4 TIR is associated with the risk of microvascular complications and can be used for assessment of glycemic control. Additionally, time below range (TBR) and time above range (TAR) are useful parameters for the evaluation of the treatment plan (Table 6.2). C
Standardized CGM Metrics for Clinical Care
| 1. Number of days CGM device is worn (recommend 14 days) | |
| 2. Percentage of time CGM device is active (recommend 70% of data from 14 days) | |
| 3. Mean glucose | |
| 4. GMI | |
| 5. Glycemic variability (%CV) target ≤36%* | |
| 6. TAR: % of readings and time >250 mg/dL (>13.9 mmol/L) | Level 2 hyperglycemia |
| 7. TAR: % of readings and time 181–250 mg/dL (10.1–13.9 mmol/L) | Level 1 hyperglycemia |
| 8. TIR: % of readings and time 70–180 mg/dL (3.9–10.0 mmol/L) | In range |
| 9. TBR: % of readings and time 54–69 mg/dL (3.0–3.8 mmol/L) | Level 1 hypoglycemia |
| 10. TBR: % of readings and time | Level 2 hypoglycemia |
| 1. Number of days CGM device is worn (recommend 14 days) | |
| 2. Percentage of time CGM device is active (recommend 70% of data from 14 days) | |
| 3. Mean glucose | |
| 4. GMI | |
| 5. Glycemic variability (%CV) target ≤36%* | |
| 6. TAR: % of readings and time >250 mg/dL (>13.9 mmol/L) | Level 2 hyperglycemia |
| 7. TAR: % of readings and time 181–250 mg/dL (10.1–13.9 mmol/L) | Level 1 hyperglycemia |
| 8. TIR: % of readings and time 70–180 mg/dL (3.9–10.0 mmol/L) | In range |
| 9. TBR: % of readings and time 54–69 mg/dL (3.0–3.8 mmol/L) | Level 1 hypoglycemia |
| 10. TBR: % of readings and time | Level 2 hypoglycemia |
Glycemic Goals
Recommendations
- 6.5a An A1C goal for many nonpregnant adults of A
- 6.5b If using AGP/GMI to assess glycemia, a parallel goal for many nonpregnant adults is TIR of >70% with TBR 50% TIR with B
- 6.6 On the basis of HCP judgment and patient preference, achievement of lower A1C levels than the goal of 7% may be acceptable and even beneficial if it can be achieved safely without significant hypoglycemia or other adverse effects of treatment. B
- 6.7 Less stringent A1C goals (such as B
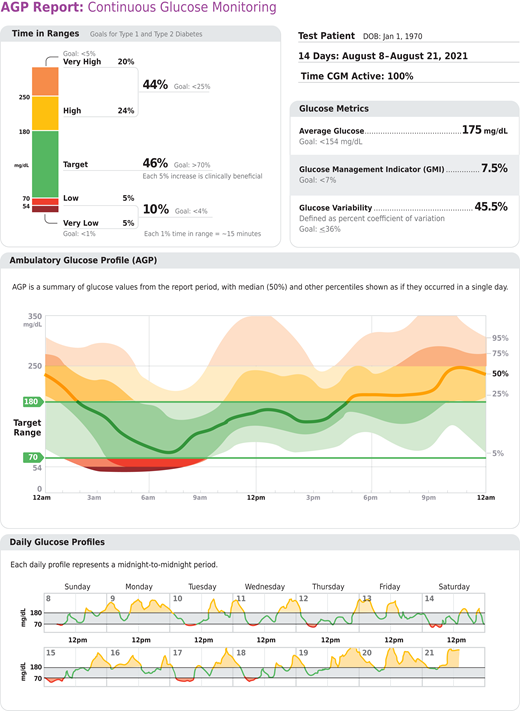
Key points included in standard AGP report. Reprinted from Holt RIG, DeVries JH, Hess-Fischl A, et al. Diabetes Care 2021;44:2589–2625.
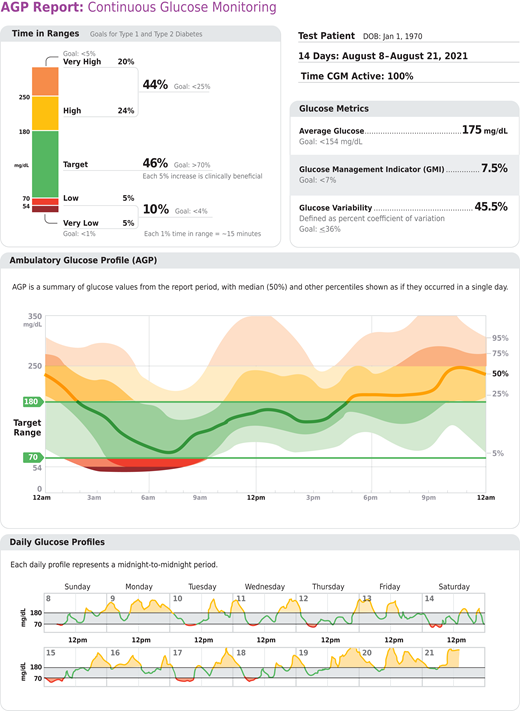
Key points included in standard AGP report. Reprinted from Holt RIG, DeVries JH, Hess-Fischl A, et al. Diabetes Care 2021;44:2589–2625.
Summary of Glycemic Recommendations for Many Nonpregnant Adults With Diabetes
| A1C | |
| Preprandial capillary plasma glucose | 80–130 mg/dL* (4.4–7.2 mmol/L) |
| Peak postprandial capillary plasma glucose† |
| A1C | |
| Preprandial capillary plasma glucose | 80–130 mg/dL* (4.4–7.2 mmol/L) |
| Peak postprandial capillary plasma glucose† |
More or less stringent glycemic goals may be appropriate for individual patients.
CGM may be used to assess glycemic target as noted in Recommendation 6.5b and Figure 6.1. Goals should be individualized based on duration of diabetes, age/life expectancy, comorbid conditions, known CVD or advanced microvascular complications, hypoglycemia unawareness, and individual patient considerations (as per Figure 6.2 in the complete 2023 Standards of Care).
Postprandial glucose may be targeted if A1C goals are not met despite reaching preprandial glucose goals. Postprandial glucose measurements should be made 1–2 hours after the beginning of the meal, generally peak levels in patients with diabetes.
Hypoglycemia
Recommendations regarding the classification of hypoglycemia are outlined in Table 6.4. See the complete 2023 Standards of Care for detailed hypoglycemia strategies.
Classification of Hypoglycemia
| . | Glycemic Criteria/Description . |
|---|---|
| Level 1 | Glucose |
| Level 2 | Glucose |
| Level 3 | A severe event characterized by altered mental and/or physical status requiring assistance for treatment of hypoglycemia |
| . | Glycemic Criteria/Description . |
|---|---|
| Level 1 | Glucose |
| Level 2 | Glucose |
| Level 3 | A severe event characterized by altered mental and/or physical status requiring assistance for treatment of hypoglycemia |
Reprinted from Agiostratidou G, Anhalt H, Ball D, et al. Diabetes Care 2017;40:1622–1630.
Recommendations
- 6.10 Occurrence and risk for hypoglycemia should be reviewed at every encounter and investigated as indicated. Awareness of hypoglycemia should be considered using validated tools. C
- 6.11 Glucose (approximately 15–20 g) is the preferred treatment for the conscious individual with blood glucose B
- 6.12 Glucagon should be prescribed for all individuals at increased risk of level 2 or 3 hypoglycemia, so that it is available should it be needed. Caregivers, school personnel, or family members providing support to these individuals should know where it is and when and how to administer it. Glucagon administration is not limited to HCPs. E
- 6.13 Hypoglycemia unawareness or one or more episodes of level 3 hypoglycemia should trigger hypoglycemia avoidance education and reevaluation and adjustment of the treatment plan to decrease hypoglycemia. E
- 6.14 Insulin-treated patients with hypoglycemia unawareness, one level 3 hypoglycemic event, or a pattern of unexplained level 2 hypoglycemia should be advised to raise their glycemic targets to strictly avoid hypoglycemia for at least several weeks in order to partially reverse hypoglycemia unawareness and reduce risk of future episodes. A
- 6.15 Ongoing assessment of cognitive function is suggested with increased vigilance for hypoglycemia by the clinician, patient, and caregivers if impaired or declining cognition is found. B
7. Diabetes Technology
Diabetes technology includes insulin delivery devices such as insulin pumps (also called continuous subcutaneous insulin infusion [CSII]) and connected insulin pens, glucose monitoring devices via CGM systems and glucose meters, automated insulin delivery (AID) systems that integrate CGM and insulin delivery with algorithms to modulate insulin delivery, and diabetes self-management support software.
General Device Principles
Recommendations
- 7.1 The type(s) and selection of devices should be individualized based on a person’s specific needs, preferences, and skill level. In the setting of an individual whose diabetes is partially or wholly managed by someone else (e.g., a young child or a person with cognitive impairment or dexterity, psychosocial, and/or physical limitations), the caregiver’s skills and preferences are integral to the decision-making process. E
- 7.2 When prescribing a device, ensure that people with diabetes/caregivers receive initial and ongoing education and training, either in-person or remotely, and ongoing evaluation of technique, results, and their ability to utilize data, including uploading/sharing data (if applicable), to monitor and adjust therapy. C
- 7.5 Initiation of CGM, CSII, and/or AID early in the treatment of diabetes can be beneficial depending on a person’s/caregiver’s needs and preferences. C
BGM
Recommendations
- 7.7 People who are on insulin using BGM should be encouraged to check their blood glucose levels when appropriate based on their insulin therapy. This may include checking when fasting, prior to meals and snacks, after meals, at bedtime, prior to exercise, when hypoglycemia is suspected, after treating low blood glucose levels until they are normoglycemic, when hyperglycemia is suspected, and prior to and while performing critical tasks such as driving. B
- 7.9 Although BGM in individuals on noninsulin therapies has not consistently shown clinically significant reductions in A1C, it may be helpful when altering nutrition plan, physical activity, and/or medications (particularly medications that can cause hypoglycemia) in conjunction with a treatment adjustment program. E
CGM Devices
Table 6.2 summarizes CGM-derived glycemic metrics, and Table 7.3 defines the available types of CGM devices.
| Type of CGM . | Description . |
|---|---|
| rtCGM | CGM systems that measure and display glucose levels continuously. |
| isCGM with and without alarms | CGM systems that measure glucose levels continuously but require scanning for visualization and storage of glucose values. |
| Professional CGM | CGM devices that are placed on the person with diabetes in the HCP’s office (or with remote instruction) and worn for a discrete period of time (generally 7–14 days). Data may be blinded or visible to the person wearing the device. The data are used to assess glycemic patterns and trends. Unlike rtCGM and isCGM devices, these devices are clinic-based and not owned by the person with diabetes. |
| Type of CGM . | Description . |
|---|---|
| rtCGM | CGM systems that measure and display glucose levels continuously. |
| isCGM with and without alarms | CGM systems that measure glucose levels continuously but require scanning for visualization and storage of glucose values. |
| Professional CGM | CGM devices that are placed on the person with diabetes in the HCP’s office (or with remote instruction) and worn for a discrete period of time (generally 7–14 days). Data may be blinded or visible to the person wearing the device. The data are used to assess glycemic patterns and trends. Unlike rtCGM and isCGM devices, these devices are clinic-based and not owned by the person with diabetes. |
Recommendations
- 7.11 Real-time CGM (rtCGM) A or intermittently scanned CGM (isCGM) B should be offered for diabetes management in adults with diabetes on multiple daily injections (MDI) or CSII who are capable of using the devices safely (either by themselves or with a caregiver). The choice of device should be made based on the individual’s circumstances, preferences, and needs.
- 7.12 rtCGM A or isCGM C should be offered for diabetes management in adults with diabetes on basal insulin who are capable of using the devices safely (either by themselves or with a caregiver). The choice of device should be made based on the individual’s circumstances, preferences, and needs.
- 7.15 In people with diabetes on MDI or CSII, rtCGM devices should be used as close to daily as possible for maximal benefit. A isCGM devices should be scanned frequently, at a minimum once every 8 hours. A People with diabetes should have uninterrupted access to their supplies to minimize gaps in CGM. A
- 7.17 Periodic use of rtCGM or isCGM or use of professional CGM can be helpful for diabetes management in circumstances where continuous use of CGM is not appropriate, desired, or available. C
- 7.18 Skin reactions, either due to irritation or allergy, should be assessed and addressed to aid in successful use of devices. E
Inpatient Care
Recommendation
- 7.30 People with diabetes who are competent to safely use diabetes devices such as insulin pumps and CGM systems should be supported to continue using them in an inpatient setting or during outpatient procedures, once competency is established and proper supervision is available. E
Other Technologies
See “7. Diabetes Technologies” in the complete 2023 Standards of Care for more information on insulin delivery systems, including insulin syringes, pens, connected pens, pumps, and AID systems; software systems; and digital health systems that combine technology with online or virtual coaching.
An ADA resource available at consumerguide.diabetes. org can help HCPs and people with diabetes make decisions as to the initial choice of devices. Other sources, including HCPs and device manufacturers, can help people troubleshoot when difficulties arise.
8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes
Strong evidence exists that obesity management can delay the progression from prediabetes to type 2 diabetes and is highly beneficial in treating type 2 diabetes.
Assessment
Recommendations
- 8.1 Use person-centered, nonjudgmental language that fosters collaboration between individuals and HCPs, including person-first language (e.g., “person with obesity” rather than “obese person”). E
- 8.2 Measure height and weight and calculate BMI at annual visits or more frequently. Assess weight trajectory to inform treatment considerations. E
- 8.5 Individuals with diabetes and overweight or obesity may benefit from modest or larger magnitudes of weight loss. Relatively small weight loss (approximately 3–7% of baseline weight) improves glycemia and other intermediate CV risk factors. A Larger, sustained weight losses (>10%) usually confer greater benefits, including disease-modifying effects and possible remission of type 2 diabetes, and may improve long-term CV outcomes and mortality. B
Nutrition, Physical Activity, and Behavioral Therapy
Recommendations
- 8.6 Nutrition, physical activity, and behavioral therapy to achieve and maintain ≥5% weight loss are recommended for most people with type 2 diabetes and overweight or obesity. Additional weight loss usually results in further improvements in the management of diabetes and CV risk. B
- 8.7 Such interventions should include a high frequency of counseling (≥16 sessions in 6 months) and focus on nutrition changes, physical activity, and behavioral strategies to achieve a 500–750 kcal/day energy deficit. A
- 8.10 Evaluate systemic, structural, and socioeconomic factors that may impact nutrition patterns and food choices, such as food insecurity and hunger, access to healthful food options, cultural circumstances, and SDOH. C
- 8.11 For those who achieve weight loss goals, long-term (≥1 year) weight maintenance programs are recommended when available. Such programs should, at minimum, provide monthly contact and support, recommend ongoing monitoring of body weight (weekly or more frequently) and other self-monitoring strategies, and encourage regular physical activity (200–300 minutes/week). A
- 8.12 Short-term nutrition intervention using structured, very-low-calorie meals (800–1,000 kcal/day) may be prescribed for carefully selected individuals by trained practitioners in medical settings with close monitoring. Long-term, comprehensive weight maintenance strategies and counseling should be integrated to maintain weight loss. B
Pharmacotherapy
Recommendations
- 8.16 Obesity pharmacotherapy is effective as an adjunct to nutrition, physical activity, and behavioral counseling for selected people with type 2 diabetes and BMI ≥27 kg/m 2 . Potential benefits and risks must be considered. A
- 8.17 If obesity pharmacotherapy is effective (typically defined as ≥5% weight loss after 3 months’ use), further weight loss is likely with continued use. When early response is insufficient (typically A
Medications for Lowering Glucose, Summary of Characteristics
*For agent-specific dosing recommendations, please refer to manufacturers’ prescribing information. 1 Tsapas A, Avgerinos I, Karagiannis T, et al. Ann Intern Med 2020;173:278–286. 2 Tsapas A, Karagiannis T, Kakotrichi P, et al. Diabetes Obes Metab 2021;23:2116–2124. CVOT, cardiovascular outcomes trial; GIP, gastric inhibitory polypeptide; GLP-1 RA, glucagon-like peptide 1 receptor agonist; NASH, nonalcoholic steatohepatitis; SQ, subcutaneous; T2DM, type 2 diabetes mellitus. Reprinted from Davies MJ, Aroda VR, Collins BS, et al. Diabetes Care 2022;45:2753–2786.
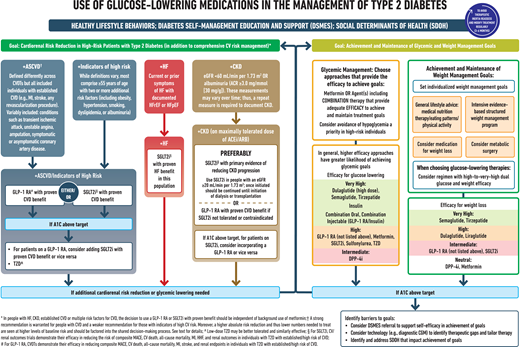
Use of glucose-lowering medications in the management of type 2 diabetes. ACEi, ACE inhibitor; ACR, albumin-to-creatinine ratio; CVOT, cardiovascular outcomes trial; DPP-4i, dipeptidyl peptidase 4 inhibitor; GLP-1 RA, glucagon-like peptide 1 receptor agonist; HHF, hospitalization for heart failure; SGLT2i, sodium-glucose cotransporter 2 inhibitor; T2D, type 2 diabetes. Adapted from Davies MJ, Aroda VR, Collins BS, et al. Diabetes Care 2022;45:2753–2786.
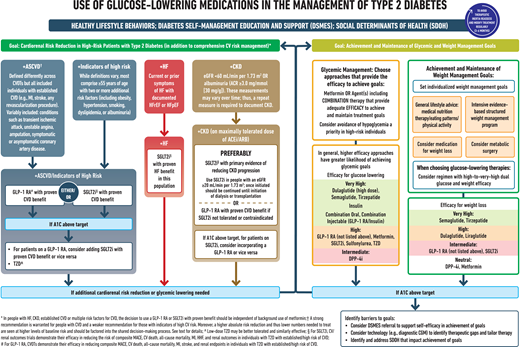
Use of glucose-lowering medications in the management of type 2 diabetes. ACEi, ACE inhibitor; ACR, albumin-to-creatinine ratio; CVOT, cardiovascular outcomes trial; DPP-4i, dipeptidyl peptidase 4 inhibitor; GLP-1 RA, glucagon-like peptide 1 receptor agonist; HHF, hospitalization for heart failure; SGLT2i, sodium-glucose cotransporter 2 inhibitor; T2D, type 2 diabetes. Adapted from Davies MJ, Aroda VR, Collins BS, et al. Diabetes Care 2022;45:2753–2786.
Approved Obesity Pharmacotherapy Options
Medications approved by the FDA for the treatment of obesity are summarized in Table 8.2 of the complete 2023 Standards of Care. Nearly all of these medications can improve glycemia in addition to weight loss for people with type 2 diabetes.
Metabolic Surgery
Recommendations
- 8.18 Metabolic surgery should be a recommended option to treat type 2 diabetes in screened surgical candidates with BMI ≥40 kg/m 2 (BMI ≥37.5 kg/m 2 in Asian American individuals) and in adults with BMI 35.0–39.9 kg/m 2 (32.5–37.4 kg/m 2 in Asian American individuals) who do not achieve durable weight loss and improvement in comorbidities (including hyperglycemia) with nonsurgical methods. A
- 8.19 Metabolic surgery may be considered as an option to treat type 2 diabetes in adults with BMI 30.0–34.9 kg/m 2 (27.5–32.4 kg/m 2 in Asian American individuals) who do not achieve durable weight loss and improvement in comorbidities (including hyperglycemia) with nonsurgical methods. A
- 8.21 People being considered for metabolic surgery should be evaluated for comorbid psychological conditions and social and situational circumstances that have the potential to interfere with surgery outcomes. B
- 8.22 People who undergo metabolic surgery should receive long-term medical and behavioral support and routine micronutrient, nutritional, and metabolic status monitoring. B
9. Pharmacologic Approaches to Glycemic Treatment
Pharmacologic Therapy for Adults With Type 1 Diabetes
See “9. Pharmacologic Approaches to Glycemic Treatment” in the complete 2023 Standards of Care for detailed information on pharmacologic approaches to type 1 diabetes management.
Pharmacologic Therapy for Adults With Type 2 Diabetes
Figure 9.3 and Table 9.2 provide details for informed decision-making on pharmacologic agents for type 2 diabetes.
Recommendations
- 9.4a Healthy lifestyle behaviors, DSMES, avoidance of clinical inertia, and SDOH should be considered in the glucose-lowering management of type 2 diabetes. Pharmacologic therapy should be guided by person-centered treatment factors, including comorbidities and treatment goals. A
- 9.4b In adults with type 2 diabetes and established/high risk of atherosclerotic cardiovascular disease (ASCVD), heart failure (HF), and/or chronic kidney disease (CKD), the treatment regimen should include agents that reduce cardiorenal risk. A
- 9.4c Pharmacologic approaches that provide adequate efficacy to achieve and maintain treatment goals should be considered, such as metformin or other agents, including combination therapy. A
- 9.4d Weight management is an impactful component of glucose-lowering management in type 2 diabetes. The glucose-lowering treatment regimen should consider approaches that support weight management goals. A
- 9.5 Metformin should be continued upon initiation of insulin therapy (unless contraindicated or not tolerated) for ongoing glycemic and metabolic benefits. A
- 9.6 Early combination therapy can be considered in some individuals at treatment initiation to extend the time to treatment failure. A
- 9.7 The early introduction of insulin should be considered if there is evidence of ongoing catabolism (weight loss), if symptoms of hyperglycemia are present, or when A1C levels (>10% [86 mmol/mol]) or blood glucose levels (≥300 mg/dL [16.7 mmol/L]) are very high. E
- 9.8 A person-centered approach should guide the choice of pharmacologic agents. Consider the effects on CV and renal comorbidities, efficacy, hypoglycemia risk, impact on weight, cost and access, risk for side effects, and individual preferences. E
- 9.9 Among individuals with type 2 diabetes who have established ASCVD or indicators of high CV risk, established kidney disease, or HF, a sodium–glucose cotransporter 2 (SGLT2) inhibitor and/or glucagon-like peptide 1 (GLP-1) receptor agonist with demonstrated CVD benefit (Figure 9.3, Table 9.2, and Tables 10.3B and 10.3C in the complete 2023 Standards of Care) is recommended as part of the glucose-lowering regimen and comprehensive CV risk reduction, independent of A1C and in consideration of person-specific factors. (See “10. CVD AND RISK MANAGEMENT,” for details on CV risk reduction recommendations). A
- 9.10 In adults with type 2 diabetes, a GLP-1 receptor agonist is preferred to insulin when possible. A
- 9.11 If insulin is used, combination therapy with a GLP-1 receptor agonist is recommended for greater efficacy, durability of treatment effect, and weight and hypoglycemia benefit. A
- 9.13 Medication regimen and medication-taking behavior should be reevaluated at regular intervals (every 3–6 months) and adjusted as needed to incorporate specific factors that impact choice of treatment (Figure 4.1 and Table 9.2). E
- 9.14 Clinicians should be aware of the potential for overbasalization with insulin therapy. Clinical signals that may prompt evaluation of overbasalization include basal dose more than ∼0.5 units/kg/day, high bedtime–morning or post- to preprandial glucose differential, hypoglycemia (aware or unaware), and high glycemic variability. Indication of overbasalization should prompt reevaluation to further individualize therapy. E
10. CVD and Risk Management
ASCVD—defined as coronary heart disease, cerebrovascular disease, or peripheral arterial disease (PAD) presumed to be of atherosclerotic origin—is the leading cause of morbidity and mortality for individuals with diabetes. Controlling individual CV risk factors helps prevent or slow ASCVD in people with diabetes. HF is another major cause of morbidity and mortality from CVD.
Risk factors, including obesity/overweight, hypertension, dyslipidemia, smoking, family history of premature coronary disease, CKD, and the presence of albuminuria, should be assessed at least annually to prevent and manage both ASCVD and HF.
The Risk Calculator
The American College of Cardiology/American Heart Association ASCVD risk calculator (Risk Estimator Plus) is generally a useful tool to estimate 10-year risk of a first ASCVD event (available online at tools.acc.org/ASCVD-Risk-Estimator-Plus).
Hypertension/BP Control
Hypertension, defined as a systolic BP ≥130 mmHg or a diastolic BP ≥80 mmHg, is common among people with either type 1 or type 2 diabetes.
Screening and Diagnosis
Recommendations
- 10.1 BP should be measured at every routine clinical visit. When possible, individuals found to have elevated BP (systolic BP 120–129 mmHg and diastolic A Hypertension is defined as a systolic BP ≥130 mmHg or a diastolic BP ≥80 mmHg based on an average of ≥2 measurements obtained on ≥2 occasions. A Individuals with BP ≥180/110 mmHg and CVD could be diagnosed with hypertension at a single visit. E
- 10.2 All people with hypertension and diabetes should monitor their BP at home. A
Treatment Goals
Recommendations
- 10.3 For people with diabetes and hypertension, BP targets should be individualized through a shared decision-making process that addresses CV risk, potential adverse effects of antihypertensive medications, and patient preferences. B
- 10.4 People with diabetes and hypertension qualify for antihypertensive drug therapy when the BP is persistently elevated ≥130/80 mmHg. The on-treatment target BP goal is B
Treatment Strategies
Lifestyle Intervention
Recommendation
- 10.6 For people with BP >120/80 mmHg, lifestyle intervention consists of weight loss when indicated, a Dietary Approaches to Stop Hypertension (DASH)-style eating pattern including reducing sodium and increasing potassium intake, moderation of alcohol intake, and increased physical activity. A
Pharmacologic Interventions
Recommendations
- 10.8 Individuals with confirmed office-based BP ≥160/100 mmHg should, in addition to lifestyle therapy, have prompt initiation and timely titration of two drugs or a single-pill combination of drugs demonstrated to reduce CV events in people with diabetes. A
- 10.10 Multiple-drug therapy is generally required to achieve BP targets. However, combinations of ACE inhibitors and angiotensin receptor blockers (ARBs) and combinations of ACE inhibitors or ARBs with direct renin inhibitors should not be used. A
- 10.11 An ACE inhibitor or ARB, at the maximum tolerated dose indicated for BP treatment, is the recommended first-line treatment for hypertension in people with diabetes and urinary albumin-to-creatinine ratio (UACR) ≥300 mg/g creatinine A or 30–299 mg/g creatinine. B If one class is not tolerated, the other should be substituted. B
- 10.12 For patients treated with an ACE inhibitor, ARB, or diuretic, serum creatinine/estimated glomerular filtration rate (eGFR) and serum potassium levels should be monitored at least annually. B
Resistant Hypertension
Recommendation
- 10.13 Individuals with hypertension who are not meeting BP targets on three classes of antihypertensive medications (including a diuretic) should be considered for mineralocorticoid receptor antagonist (MRA) therapy. A
Lipid Management
Lifestyle Intervention
Recommendations
- 10.14 Lifestyle modification focusing on weight loss (if indicated); application of a Mediterranean or DASH eating pattern; reduction of saturated fat and trans fat; increase of dietary n-3 fatty acids, viscous fiber, and plant stanols/sterols intake; and increased physical activity should be recommended to improve the lipid profile and reduce the risk of developing ASCVD in people with diabetes. A
- 10.15 Intensify lifestyle therapy and optimize glycemic control for patients with elevated triglyceride levels (≥150 mg/dL [1.7 mmol/L]) and/or low HDL cholesterol (C
Ongoing Therapy and Monitoring With Lipid Panel
Recommendations
- 10.16 In adults not taking statins or other lipid-lowering therapy, it is reasonable to obtain a lipid profile at the time of diabetes diagnosis, at an initial medical evaluation, and every 5 years thereafter if under the age of 40 years, or more frequently if indicated. E
- 10.17 Obtain a lipid profile at initiation of statins or other lipid-lowering therapy, 4–12 weeks after initiation or a change in dose, and annually thereafter, as it may help to monitor the response to therapy and inform medication taking. E
Statin Treatment
Primary Prevention
Recommendations
- 10.18 For people with diabetes aged 40–75 years without ASCVD, use moderate-intensity statin therapy in addition to lifestyle therapy. A
- 10.19 For people with diabetes aged 20–39 years with additional ASCVD risk factors, it may be reasonable to initiate statin therapy in addition to lifestyle therapy. C
- 10.20 For people with diabetes aged 40–75 at higher CV risk, including those with one or more ASCVD risk factors, it is recommended to use high-intensity statin therapy to reduce LDL cholesterol by ≥50% of baseline and to target an LDL cholesterol goal of B
- 10.21 For people with diabetes aged 40–75 years at higher CV risk, especially those with multiple ASCVD risk factors and an LDL cholesterol ≥70 mg/dL, it may be reasonable to add ezetimibe or a PCSK9 inhibitor to maximum tolerated statin therapy. C
- 10.22 In adults with diabetes aged >75 years already on statin therapy, it is reasonable to continue statin treatment. B
- 10.23 In adults with diabetes aged >75 years, it may be reasonable to initiate moderate-intensity statin therapy after discussion of potential benefits and risks. C
Secondary Prevention
Recommendations
- 10.25 For people of all ages with diabetes and ASCVD, high-intensity statin therapy should be added to lifestyle therapy. A
- 10.26 For people with diabetes and ASCVD, treatment with high-intensity statin therapy is recommended to target an LDL cholesterol reduction of ≥50% from baseline and an LDL cholesterol goal of B
- 10.27 For individuals who do not tolerate the intended intensity, the maximum tolerated statin dose should be used. E
Treatment of Other Lipoprotein Fractions or Targets
Recommendations
- 10.28 For individuals with fasting triglyceride levels ≥500 mg/dL, evaluate for secondary causes of hypertriglyceridemia and consider medical therapy to reduce the risk of pancreatitis. C
- 10.29 In adults with moderate hypertriglyceridemia (fasting or nonfasting triglycerides 175–499 mg/dL), clinicians should address and treat lifestyle factors (obesity and metabolic syndrome), secondary factors (diabetes, chronic liver or kidney disease and/or nephrotic syndrome, hypothyroidism), and medications that raise triglycerides. C
- 10.30 In individuals with ASCVD or other CV risk factors on a statin with controlled LDL cholesterol but elevated triglycerides (135–499 mg/dL), the addition of icosapent ethyl can be considered to reduce CV risk. A
Other Combination Therapy
Recommendations
- 10.31 Statin plus fibrate combination therapy has not been shown to improve ASCVD and is generally not recommended. A
- 10.32 Statin plus niacin combination therapy has not been shown to provide additional CV benefit above statin therapy alone, may increase the risk of stroke with additional side effects, and is generally not recommended. A
Lipid-Lowering Agents and Cognitive Function
The concern that lipid-lowering agents may adversely affect cognitive function is not currently supported by evidence and should not deter their use.
Antiplatelet Agents
Recommendations
- 10.33 Use aspirin therapy (75–162 mg/day) as a secondary prevention strategy in those with diabetes and a history of ASCVD. A
- 10.34 For individuals with ASCVD and documented aspirin allergy, clopidogrel (75 mg/day) should be used. B
- 10.35 Dual antiplatelet therapy (with low-dose aspirin and a P2Y12 inhibitor) is reasonable for a year after an acute coronary syndrome and may have benefits beyond this period. A
- 10.36 Long-term treatment with dual antiplatelet therapy should be considered for individuals with prior coronary intervention, high ischemic risk, and low bleeding risk to prevent major adverse cardiovascular events (MACE). A
- 10.37 Combination therapy with aspirin plus low-dose rivaroxaban should be considered for individuals with stable CAD and/or PAD and low bleeding risk to prevent major adverse limb and CV events. A
- 10.38 Aspirin therapy (75–162 mg/day) may be considered as a primary prevention strategy in those with diabetes who are at increased CV risk, after a comprehensive discussion with the patient on the benefits versus the comparable increased risk of bleeding. A
CVD
Screening
Recommendations
- 10.39 In asymptomatic individuals, routine screening for CAD is not recommended as it does not improve outcomes as long as ASCVD risk factors are treated. A
- 10.40 Consider investigations for CAD in the presence of any of the following: atypical cardiac symptoms (e.g., unexplained dyspnea, chest discomfort); signs or symptoms of associated vascular disease including carotid bruits, transient ischemic attack, stroke, claudication, or PAD; or electrocardiogram (ECG) abnormalities (e.g., Q waves). E
Treatment
Recommendations
- 10.41 Among people with type 2 diabetes who have established ASCVD or established kidney disease, an SGLT2 inhibitor or GLP-1 receptor agonist with demonstrated CVD benefit (see Tables 10.3B and 10.3C in the complete 2023 Standards of Care) is recommended as part of the comprehensive CV risk reduction and/or glucose-lowering regimens. A
- 10.41a In people with type 2 diabetes and established ASCVD, multiple ASCVD risk factors, or diabetic kidney disease (DKD), an SGLT2 inhibitor with demonstrated CV benefit is recommended to reduce the risk of MACE and/or HF hospitalization. A
- 10.41b In people with type 2 diabetes and established ASCVD or multiple risk factors for ASCVD, a GLP-1 receptor agonist with demonstrated CV benefit is recommended to reduce the risk of MACE. A
- 10.41c In people with type 2 diabetes and established ASCVD or multiple risk factors for ASCVD, combined therapy with an SGLT2 inhibitor with demonstrated CV benefit and a GLP-1 receptor agonist with demonstrated CV benefit may be considered for additive reduction in the risk of adverse CV and kidney events. A
- 10.42a In people with type 2 diabetes and established HF with either preserved ejection fraction (HFpEF) or reduced ejection fraction (HFrEF), an SGLT2 inhibitor with proven benefit in this patient population is recommended to reduce risk of worsening HF and CV death. A
- 10.42b In people with type 2 diabetes and established HF with either HFpEF or HFrEF, an SGLT2 inhibitor with proven benefit in this patient population is recommended to improve symptoms, physical limitations, and QoL. A
- 10.43 For people with type 2 diabetes and CKD with albuminuria treated with maximum tolerated doses of ACE inhibitor or ARB, addition of finerenone is recommended to improve CV outcomes and reduce the risk of CKD progression. A
- 10.44 In people with known ASCVD, particularly CAD, ACE inhibitor or ARB therapy is recommended to reduce the risk of CV events. A
- 10.45 In people with prior MI, β-blockers should be continued for 3 years after the event. B
- 10.46 Treatment of individuals with HFrEF should include a β-blocker with proven CV outcomes benefit, unless otherwise contraindicated. A
- 10.47 In people with type 2 diabetes with stable HF, metformin may be continued for glucose lowering if eGFR remains >30 mL/min/1.73 m 2 but should be avoided in unstable or hospitalized individuals with HF. B
11. CKD and Risk Management
CKD
Optimize glucose and BP control and reduce BP variability to reduce the risk or slow the progression of CKD.
Screening
Recommendations
- 11.1a At least annually, urinary albumin (e.g., spot UACR) and eGFR should be assessed in people with type 1 diabetes with duration of ≥5 years and in all people with type 2 diabetes regardless of treatment. B
- 11.1b In people with established DKD, urinary albumin (e.g., spot UACR) and eGFR should be monitored 1–4 times per year depending on the stage of the disease (see Figure 11.1 in the complete 2023 Standards of Care). B
Treatment
Recommendations
- 11.4a In nonpregnant people with diabetes and hypertension, either an ACE inhibitor or an ARB is recommended for those with moderately increased albuminuria (UACR 30–299 mg/g creatinine) B and is strongly recommended for those with severely increased albuminuria (UACR ≥300 mg/g creatinine) and/or eGFR A
- 11.4b Periodically monitor serum creatinine and potassium levels for the development of increased creatinine and hyperkalemia when ACE inhibitors, ARBs, and MRAs are used, or hypokalemia when diuretics are used. B
- 11.4c An ACE inhibitor or an ARB is not recommended for the primary prevention of CKD in people with diabetes who have normal BP, normal UACR (A
- 11.4d Do not discontinue renin-angiotensin system blockade for increases in serum creatinine (≤30%) in the absence of volume depletion. A
- 11.5a For people with type 2 diabetes and DKD, use of an SGLT2 inhibitor is recommended to reduce CKD progression and CV events in patients with an eGFR ≥20 mL/min/1.73 m 2 and urinary albumin ≥200 mg/g creatinine. A
- 11.5b For people with type 2 diabetes and DKD, use of an SGLT2 inhibitor is recommended to reduce CKD progression and CV events in patients with an eGFR ≥20 mL/min/1.73 m 2 and urinary albumin ranging from normal to 200 mg/g creatinine. B
- 11.5c In people with type 2 diabetes and DKD, consider use of SGLT2 inhibitors (if eGFR is ≥20 mL/min/1.73 m 2 ), a GLP-1 receptor agonist, or a nonsteroidal MRA (if eGFR is ≥25 mL/min/1.73 m 2 ) additionally for CV risk reduction. A
- 11.5d In people with CKD and albuminuria who are at increased risk for CV events or CKD progression, a nonsteroidal MRA shown to be effective in clinical trials is recommended to reduce CKD progression and CV events. A
- 11.6 In people with CKD who have ≥300 mg/g urinary albumin, a reduction of 30% or greater in mg/g urinary albumin is recommended to slow CKD progression. B
- 11.7 For people with non–dialysis-dependent stage 3 or higher CKD, dietary protein intake should be aimed to a target level of 0.8 g/kg body weight per day. A For patients on dialysis, higher levels of dietary protein intake should be considered since protein energy wasting is a major problem in some individuals on dialysis. B
- 11.8 Patients should be referred for evaluation by a nephrologist if they have continuously increasing urinary albumin levels and/or continuously decreasing eGFR and if the eGFR is A
- 11.9 Promptly refer to a nephrologist for uncertainty about the etiology of kidney disease, difficult management issues, and rapidly progressing kidney disease. A
Diagnosis, Staging, and Surveillance of DKD
DKD is diagnosed based on the presence and degree of albuminuria and/or reduced eGFR in the absence of symptoms of other primary causes of kidney damage. Two of three specimens of UACR collected within a 3- to 6-month period should be abnormal before considering a patient to have albuminuria. eGFR should be calculated from serum creatinine using a validated formula. The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation is generally preferred. Race should not be included in the formula as race is a social and not a biologic construct. CKD is staged as detailed in Figure 11.1 in the complete 2023 Standards of Care.
Selection of Glucose-Lowering Medications for People With CKD
See Table 9.2 for general drug-specific factors, including adverse event information, for antihyperglycemic agents.
Nonsteroidal MRAs in CKD
Finerenone can reduce DKD, CV events, and HF hospitalization in people with advanced DKD, but it should be used with caution due to a risk of hyperkalemia. It can be used with SGLT2 inhibitors.
12. Retinopathy, Neuropathy, and Foot Care
Management of glycemia, BP, and lipids can reduce the risk or slow the progression of microvascular complications of diabetes.
Diabetic Retinopathy
Screening
Recommendations
- 12.4 People with type 2 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist at the time of the diabetes diagnosis. B
- 12.5 If there is no evidence of diabetic retinopathy (DR) for one or more annual eye exams and glycemia is well controlled, then screening every 1–2 years may be considered. If any level of DR is present, subsequent dilated retinal examinations should be repeated at least annually by an ophthalmologist or optometrist. If DR is progressing or sight-threatening, then examinations will be required more frequently. B
- 12.6 Programs that use retinal photography (with remote reading or use of a validated assessment tool) to improve access to DR screening can be appropriate screening strategies for DR. Such programs need to provide pathways for timely referral for a comprehensive eye examination when indicated. B
Treatment
Recommendations
- 12.9 Promptly refer individuals with any level of diabetic macular edema, moderate or worse nonproliferative DR (a precursor of proliferative DR), or any proliferative DR to an ophthalmologist who is knowledgeable and experienced in the management of DR. A
- 12.14 The presence of DR is not a contraindication to aspirin therapy for cardioprotection, as aspirin does not increase the risk of retinal hemorrhage. A
Neuropathy
Screening
Recommendations
- 12.15 All people with diabetes should be assessed for diabetic peripheral neuropathy (DPN) starting at diagnosis of type 2 diabetes and 5 years after the diagnosis of type 1 diabetes and at least annually thereafter. B
- 12.16 Assessment for distal symmetric polyneuropathy should include a careful history and assessment of either temperature or pinprick sensation (small-fiber function) and vibration sensation using a 128-Hz tuning fork (for large-fiber function). All people with diabetes should have annual 10-g monofilament testing to identify feet at risk for ulceration and amputation. B
- 12.17 Symptoms and signs of autonomic neuropathy should be assessed in people with diabetes starting at diagnosis of type 2 diabetes and 5 years after the diagnosis of type 1 diabetes and at least annually thereafter and with evidence of other microvascular complications, particularly kidney disease and DPN. Screening can include asking about orthostatic dizziness, syncope, or dry cracked skin in the extremities. Signs of autonomic neuropathy include orthostatic hypotension, a resting tachycardia, or evidence of peripheral dryness or cracking of skin. E
Treatment
Recommendation
- 12.20 Gabapentinoids, serotonin-norepinephrine reuptake inhibitors, tricyclic antidepressants, and sodium channel blockers are recommended as initial pharmacologic treatments for neuropathic pain in diabetes. A Refer to neurologist or pain specialist when pain control is not achieved within the scope of practice of the treating physician. E
Foot Care
Recommendations
- 12.21 Perform a comprehensive foot evaluation at least annually to identify risk factors for ulcers and amputations. A
- 12.22 The examination should include inspection of the skin, assessment of foot deformities, neurological assessment (10-g monofilament testing with at least one other assessment: pinprick, temperature, vibration), and vascular assessment, including pulses in the legs and feet. B
- 12.23 Individuals with evidence of sensory loss or prior ulceration or amputation should have their feet inspected at every visit. A
- 12.24 Obtain a prior history of ulceration, amputation, Charcot foot, angioplasty or vascular surgery, cigarette smoking, retinopathy, and renal disease and assess current symptoms of neuropathy (pain, burning, numbness) and vascular disease (leg fatigue, claudication). B
- 12.25 Initial screening for PAD should include assessment of lower-extremity pulses, capillary refill time, rubor on dependency, pallor on elevation, and venous filling time. Individuals with a history of leg fatigue, claudication, and rest pain relieved with dependency or decreased or absent pedal pulses should be referred for ankle–brachial index and for further vascular assessment as appropriate. B
- 12.26 A multidisciplinary approach is recommended for individuals with foot ulcers and high-risk feet (e.g., those on dialysis, those with Charcot foot, those with a history of prior ulcers or amputation, those with PAD). B
- 12.27 Refer individuals who smoke and have a history of prior lower-extremity complications, loss of protective sensation, structural abnormalities, or PAD to foot care specialists for ongoing preventive care and lifelong surveillance. B
- 12.28 Provide general preventive foot self-care education to all people with diabetes, including those with loss of protective sensation, on appropriate ways to examine their feet (palpation or visual inspection with an unbreakable mirror) for daily surveillance of early foot problems. B
- 12.29 The use of specialized therapeutic footwear is recommended for people with diabetes at high risk for ulceration, including those with loss of protective sensation, foot deformities, ulcers, callous formation, poor peripheral circulation, or history of amputation. B
13. Older Adults
Recommendations
- 13.1 Consider the assessment of medical, psychological, functional (self-management abilities), and social domains in older adults to provide a framework to determine targets and therapeutic approaches for diabetes management. B
- 13.2 Screen for geriatric syndromes (i.e., polypharmacy, cognitive impairment, depression, urinary incontinence, falls, persistent pain, and frailty) in older adults, as they may affect diabetes self-management and diminish QoL. B
Neurocognitive Function
Recommendation
- 13.3 Screening for early detection of mild cognitive impairment or dementia should be performed for adults 65 years of age or older at the initial visit, annually, and as appropriate. B
Hypoglycemia
Recommendations
- 13.4 Because older adults with diabetes have a greater risk of hypoglycemia than younger adults, episodes of hypoglycemia should be ascertained and addressed at routine visits. B
- 13.6 For older adults with type 2 diabetes on multiple daily doses of insulin, CGM should be considered to improve glycemic outcomes and decrease glucose variability. B
Treatment Goals
Providers caring for older adults with diabetes must take clinical, cognitive, and functional differences into consideration when setting and prioritizing treatment goals. Table 13.1 provides a treatment goal framework for older patients.
Framework for Considering Treatment Goals for Glycemia, BP, and Dyslipidemia in Older Adults With Diabetes
| Patient Characteristics/Health Status . | Rationale . | Reasonable A1C Goal‡ . | Fasting or Preprandial Glucose . | Bedtime Glucose . | BP . | Lipids . |
|---|---|---|---|---|---|---|
| Healthy (few coexisting chronic illnesses, intact cognitive and functional status) | Longer remaining life expectancy | 80–130 mg/dL (4.4–7.2 mmol/L) | 80–180 mg/dL (4.4–10.0 mmol/L) | Statin, unless contraindicated or not tolerated | ||
| Complex/intermediate (multiple coexisting chronic illnesses* or two or more instrumental ADL impairments or mild-to-moderate cognitive impairment) | Intermediate remaining life expectancy, high treatment burden, hypoglycemia vulnerability, fall risk | 90–150 mg/dL (5.0–8.3 mmol/L) | 100–180 mg/dL (5.6–10.0 mmol/L) | Statin, unless contraindicated or not tolerated | ||
| Very complex/poor health (LTC or end-stage chronic illnesses** or moderate-to-severe cognitive impairment or two or more ADL impairments) | Limited remaining life expectancy makes benefit uncertain | Avoid reliance on A1C; glucose control decisions should be based on avoiding hypoglycemia and symptomatic hyperglycemia | 100–180 mg/dL (5.6–10.0 mmol/L) | 110–200 mg/dL (6.1–11.1 mmol/L) | Consider likelihood of benefit with statin |
| Patient Characteristics/Health Status . | Rationale . | Reasonable A1C Goal‡ . | Fasting or Preprandial Glucose . | Bedtime Glucose . | BP . | Lipids . |
|---|---|---|---|---|---|---|
| Healthy (few coexisting chronic illnesses, intact cognitive and functional status) | Longer remaining life expectancy | 80–130 mg/dL (4.4–7.2 mmol/L) | 80–180 mg/dL (4.4–10.0 mmol/L) | Statin, unless contraindicated or not tolerated | ||
| Complex/intermediate (multiple coexisting chronic illnesses* or two or more instrumental ADL impairments or mild-to-moderate cognitive impairment) | Intermediate remaining life expectancy, high treatment burden, hypoglycemia vulnerability, fall risk | 90–150 mg/dL (5.0–8.3 mmol/L) | 100–180 mg/dL (5.6–10.0 mmol/L) | Statin, unless contraindicated or not tolerated | ||
| Very complex/poor health (LTC or end-stage chronic illnesses** or moderate-to-severe cognitive impairment or two or more ADL impairments) | Limited remaining life expectancy makes benefit uncertain | Avoid reliance on A1C; glucose control decisions should be based on avoiding hypoglycemia and symptomatic hyperglycemia | 100–180 mg/dL (5.6–10.0 mmol/L) | 110–200 mg/dL (6.1–11.1 mmol/L) | Consider likelihood of benefit with statin |
This table represents a consensus framework for considering treatment goals for glycemia, BP, and dyslipidemia in older adults with diabetes. The patient characteristic categories are general concepts. Not every patient will clearly fall into a particular category. Consideration of patient and caregiver preferences is an important aspect of treatment individualization. Additionally, a patient’s health status and preferences may change over time.
A lower A1C goal may be set for an individual if achievable without recurrent or severe hypoglycemia or undue treatment burden.
Coexisting chronic illnesses are conditions serious enough to require medications or lifestyle management and may include arthritis, cancer, HF, depression, emphysema, falls, hypertension, incontinence, stage 3 or worse CKD, MI, and stroke. “Multiple” means at least three, but many patients may have five or more.
The presence of a single end-stage chronic illness, such as stage 3–4 HF or oxygen-dependent lung disease, CKD requiring dialysis, or uncontrolled metastatic cancer, may cause significant symptoms or impairment of functional status and significantly reduce life expectancy. ADL, activities of daily living. Adapted from Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes Care 2012;35:2650–2664.
Lifestyle Management
Recommendations
- 13.13 Optimal nutrition and protein intake is recommended for older adults; regular exercise, including aerobic activity, weight-bearing exercise, and/or resistance training, should be encouraged in all older adults who can safely engage in such activities. B
- 13.14 For older adults with type 2 diabetes, overweight/obesity, and capacity to safely exercise, an intensive lifestyle intervention focused on dietary changes, physical activity, and modest weight loss (e.g., 5–7%) should be considered for its benefits on QoL, mobility and physical functioning, and cardiometabolic risk factor control. A
Pharmacologic Therapy
Recommendations
- 13.15 In older adults with type 2 diabetes at increased risk of hypoglycemia, medication classes with low risk of hypoglycemia are preferred. B
- 13.16 Overtreatment of diabetes is common in older adults and should be avoided. B
- 13.17 Deintensification of treatment goals is recommended to reduce the risk of hypoglycemia if it can be achieved within the individualized A1C target. B
- 13.18 Simplification of complex treatment plans (especially insulin) is recommended to reduce the risk of hypoglycemia and polypharmacy and decrease the burden of the disease if it can be achieved within the individualized A1C target. B
- 13.19 Consider costs of care and insurance coverage rules when developing treatment plans in order to reduce risk of cost-related barriers to adherence. B
Metformin is the first-line agent for older adults with type 2 diabetes, although it can cause problematic gastrointestinal side effects and vitamin B12 deficiency. Thiazolidinediones and longer-acting sulfonylureas should be avoided. Dipeptidyl peptidase 4 inhibitors are well tolerated. GLP-1 receptor agonists and SGLT2 inhibitors have CV and renal benefits that extend to older adults, although class-specific side effects may limit their use. Multiple daily insulin therapy may be too complex for many older patients. Simplification of the insulin plan to match an individual’s self-management abilities has been shown to reduce hypoglycemia and disease-related distress without worsening glycemic outcomes. Figure 13.1 in the complete 2023 Standards of Care provides an approach to insulin plan simplification.
Treatment in Skilled Nursing Facilities and Nursing Homes
Recommendations
- 13.20 Consider diabetes education for the staff of long-term care (LTC) and rehabilitation facilities to improve the management of older adults with diabetes. E
- 13.21 People with diabetes residing in LTC facilities need careful assessment to establish individualized glycemic goals and to make appropriate choices of glucose-lowering agents based on their clinical and functional status. E
- 13.22 Consider use of CGM to assess risk for hypoglycemia in older adults treated with sulfonylureas or insulin. E
End-of-Life Care
Recommendations
- 13.23 When palliative care is needed in older adults with diabetes, HCPs should initiate conversations regarding the goals and intensity of care. Strict glucose and BP control are not necessary E, and simplification of regimens can be considered. Similarly, the intensity of lipid management can be relaxed, and withdrawal of lipid-lowering therapy may be appropriate. A
- 13.24 Overall comfort, prevention of distressing symptoms, and preservation of QoL and dignity are primary goals for diabetes management at the end of life. C
14. Children and Adolescents
The management of diabetes in children and adolescents cannot simply be derived from care routinely provided to adults with diabetes. The epidemiology, pathophysiology, developmental considerations, and response to therapy in pediatric-onset diabetes are different from adult diabetes.
See “14. Children and Adolescents” in the complete 2023 Standards of Care for specific recommendations regarding the comprehensive treatment of type 1 and type 2 diabetes in children and adolescents. The ADA position statements “Type 1 Diabetes in Children and Adolescents” and “Evaluation and Management of Youth-Onset Type 2 Diabetes” provide additional information.
Type 1 Diabetes
A multidisciplinary team of specialists trained in pediatric diabetes management and sensitive to the challenges of children and adolescents with type 1 diabetes and their families, as well as the unique aspects of pediatric diabetes management, should provide care for this population.
Type 2 Diabetes
Evidence suggests that type 2 diabetes in youth is different not only from type 1 diabetes, but also from type 2 diabetes in adults, with a more rapid, progressive decline in β-cell function and accelerated development of diabetes complications.
Management
Treatment of youth-onset type 2 diabetes should include lifestyle management, diabetes self-management education, and pharmacologic treatment. Self-management in pediatric diabetes involves both the youth and their adult caregivers. Current pharmacologic treatment options for youth-onset type 2 diabetes are limited to three classes of drugs: insulin, metformin, and, in those ≥10 years of age with no contraindications, GLP-1 receptor agonists indicated for use in youth. As comorbidities may already be present at the time of diagnosis, screening and treatment of risk factors are recommended. Consideration of the sociocultural context and efforts to personalize diabetes management are of critical importance to minimize barriers to care, enhance adherence, and maximize response to treatment.
Glycemic Targets
Recommendations
Pharmacologic Management
Recommendations
- 14.66 Initiate pharmacologic therapy, in addition to behavioral counseling for healthful nutrition and physical activity changes, at diagnosis of type 2 diabetes. A
- 14.74 Use of medications not approved by the FDA for youth with type 2 diabetes is not recommended outside of research trials. B
Transition From Pediatric to Adult Care
Recommendation
- 14.111 Pediatric diabetes care teams should begin to prepare youth for transition to adult health care in early adolescence and, at the latest, at least 1 year before the transition. E
15. Management of Diabetes in Pregnancy
Diabetes confers significantly greater maternal and fetal risk largely related to the degree of hyperglycemia but also related to chronic complications and comorbidities of diabetes. In general, specific risks of diabetes in pregnancy include spontaneous abortion, fetal anomalies, preeclampsia, fetal demise, macrosomia, neonatal hypoglycemia, hyperbilirubinemia, and neonatal respiratory distress syndrome, among others. In addition, diabetes in pregnancy may increase the risk of obesity, hypertension, and type 2 diabetes in offspring later in life.
Preconception Counseling and Care
Recommendations
- 15.1 Starting at puberty and continuing in all people with diabetes and reproductive potential, preconception counseling should be incorporated into routine diabetes care. A
- 15.2 Family planning should be discussed, and effective contraception (with consideration of long-acting, reversible contraception) should be prescribed and used until an individual’s treatment plan and A1C are optimized for pregnancy. A
- 15.3 Preconception counseling should address the importance of achieving glucose levels as close to normal as is safely possible, ideally A1C A
- 15.5 In addition to focused attention on achieving glycemic targets A, standard preconception care should be augmented with extra focus on nutrition, diabetes education, and screening for diabetes comorbidities and complications. B
- 15.6 Individuals with preexisting type 1 or type 2 diabetes who are planning a pregnancy or who have become pregnant should be counseled on the risk of development and/or progression of DR. Dilated eye examinations should occur ideally before pregnancy or in the first trimester, and then pregnant individuals should be monitored every trimester and for 1 year postpartum as indicated by the degree of retinopathy and as recommended by the eye care HCP. B
Management of GDM
Recommendations
- 15.14 Lifestyle behavior change is an essential component of management of GDM and may suffice as treatment for many individuals. Insulin should be added if needed to achieve glycemic targets. A
- 15.15 Insulin is the preferred medication for treating hyperglycemia in GDM. Metformin and glyburide should not be used as first-line agents, as both cross the placenta to the fetus. A Other oral and noninsulin injectable glucose-lowering medications lack long-term safety data.
- 15.17 Telehealth visits for pregnant people with GDM improve outcomes compared with standard in-person care. A
Pregnancy and Drug Considerations
Recommendations
- 15.21 In pregnant individuals with diabetes and chronic hypertension, a BP threshold of 140/90 mmHg for initiation or titration of therapy is associated with better pregnancy outcomes than reserving treatment for severe hypertension, with no increase in risk of small-for-gestational-age birth weight. A There are limited data on the optimal lower limit, but therapy should be lessened for BP E A BP target of 110–135/85 mmHg is suggested in the interest of reducing the risk for accelerated maternal hypertension. A
- 15.22 Potentially harmful medications in pregnancy (i.e., ACE inhibitors, ARBs, statins) should be stopped prior to conception and avoided in sexually active individuals of childbearing potential who are not using reliable contraception. B
Postpartum Care
Recommendations
- 15.23 Insulin resistance decreases dramatically immediately postpartum, and insulin requirements need to be evaluated and adjusted as they are often roughly half the prepregnancy requirements for the initial few days postpartum. C
- 15.24 A contraceptive plan should be discussed and implemented with all people with diabetes of reproductive potential. A
- 15.25 Screen individuals with a recent history of GDM at 4–12 weeks postpartum, using the 75-g OGTT and clinically appropriate nonpregnancy diagnostic criteria. B
- 15.26 Individuals with overweight/obesity and a history of GDM found to have prediabetes should receive intensive lifestyle interventions and/or metformin to prevent diabetes. A
- 15.27 Breastfeeding is recommended to reduce the risk of maternal type 2 diabetes and should be considered when choosing whether to breastfeed or formula feed. B
- 15.28 Individuals with a history of GDM should have lifelong screening for the development of type 2 diabetes or prediabetes every 1–3 years. B
- 15.30 Postpartum care should include psychosocial assessment and support for self-care. E
16. Diabetes Care in the Hospital
Among hospitalized individuals, hyperglycemia, hypoglycemia, and glucose variability are associated with adverse outcomes, including death. Therefore, careful management of people with diabetes during hospitalization has direct and immediate benefits. When caring for hospitalized people with diabetes, consult with a specialized diabetes or glucose management team when possible.
Hospital Care Delivery Standards
Recommendations
- 16.1 Perform an A1C test on all people with diabetes or hyperglycemia (blood glucose >140 mg/dL [7.8 mmol/L]) admitted to the hospital if not performed in the prior 3 months. B
- 16.2 Insulin should be administered using validated written or computerized protocols that allow for predefined adjustments in the insulin dosage based on glycemic fluctuations. B
Glycemic Targets in Hospitalized Adults
Recommendations
- 16.4 Insulin therapy should be initiated for the treatment of persistent hyperglycemia starting at a threshold ≥180 mg/dL (10.0 mmol/L) (checked on two occasions). Once insulin therapy is started, a target glucose range of 140–180 mg/dL (7.8–10.0 mmol/L) is recommended for most critically ill and noncritically ill patients. A
- 16.5 More stringent goals, such as 110–140 mg/dL (6.1–7.8 mmol/L) or 100–180 mg/dL (5.6–10.0 mmol/L), may be appropriate for selected patients and are acceptable if they can be achieved without significant hypoglycemia. C
BGM
In hospitalized individuals with diabetes who are eating, point-of-care (POC) glucose monitoring should be performed before meals; in those not eating, glucose monitoring is advised every 4–6 hours. Although CGM has theoretical advantages over POC glucose monitoring in detecting and reducing the incidence of hypoglycemia, it has not been approved by the FDA for inpatient use.
Glucose-Lowering Treatment in Hospitalized Patients
Recommendations
- 16.6 Basal insulin or a basal plus bolus correction insulin regimen is the preferred treatment for noncritically ill hospitalized patients with poor oral intake or those who are taking nothing by mouth. A
- 16.7 An insulin regimen with basal, prandial, and correction components is the preferred treatment for most noncritically ill hospitalized patients with adequate nutritional intake. A
- 16.8 Use of a correction or supplemental insulin without basal insulin (often referred to as a sliding scale) in the inpatient setting is discouraged. A
Insulin Therapy
In the critical care setting, continuous intravenous insulin infusion is the most effective method for achieving glycemic targets. When discontinuing intravenous insulin, a transition protocol is associated with less morbidity and lower costs of care.
In the noncritical care setting, insulin is the preferred treatment for hyperglycemia. However, in certain circumstances, it may be appropriate to continue home therapies, including oral glucose-lowering medications. The safety and efficacy of noninsulin glucose-lowering therapies in the hospital setting is an area of active research. (See “16. Diabetes Care in the Hospital” in the complete 2023 Standards of Care for details.) If oral medications are held in the hospital but will be reinstated after discharge, there should be a protocol for guiding resumption of home medications 1–2 days prior to discharge.
An insulin schedule with basal and correction components is necessary for all hospitalized individuals with type 1 diabetes, even when taking nothing by mouth, with the addition of prandial insulin when eating.
Hypoglycemia
Recommendations
- 16.9 A hypoglycemia management protocol should be adopted and implemented by each hospital or hospital system. A plan for preventing and treating hypoglycemia should be established for each individual. Episodes of hypoglycemia in the hospital should be documented in the medical record and tracked for quality improvement/quality assessment. E
- 16.10 Treatment regimens should be reviewed and changed as necessary to prevent further hypoglycemia when a blood glucose value of C
Insulin is one of the most common drugs causing adverse events in hospitalized patients, and errors in insulin dosing and/or administration occur relatively frequently.
MNT in the Hospital
The goals of MNT in the hospital are to provide adequate calories to meet metabolic demands, optimize glycemic outcomes, address personal food preferences, and facilitate the creation of a discharge plan.
Self-Management in the Hospital
Diabetes self-management in the hospital may be appropriate for specific individuals who wish to continue to perform self-care while acutely ill.
Standards for Special Situations
See “16. DIABETES CARE IN THE HOSPITAL” in the complete 2023 Standards of Care for guidance on enteral/parenteral feedings, glucocorticoid therapy, perioperative care, and DKA and hyperosmolar hyperglycemic state.
Transition From the Hospital to the Ambulatory Setting
Recommendation
- 16.11 A structured discharge plan should be tailored to the individual with diabetes. B
Preventing Admissions and Readmissions
People with diabetes are nearly twice as likely as those without diabetes to be readmitted after hospitalization. Strategies to reduce readmissions include targeting ketosis-prone type 1 diabetes, treating individuals with admission A1C >9% (75 mmol/mol) with insulin, and implementing a transitional care model.
17. Diabetes Advocacy
For a list of ADA advocacy position statements, including “Diabetes and Driving” and “Diabetes and Employment,” see “17. Diabetes Advocacy” in the complete 2023 Standards of Care.
Article Information
Acknowledgments
This abridged version of the Standards of Care in Diabetes—2023 was created by the ADA’s Primary Care Advisory Group (PCAG), with special thanks to PCAG chair Hope Feldman, CRNP, FNP-BC, of Philadelphia, PA; ADA lead Nuha Ali ElSayed, MD, MMSc; Rozalina G. McCoy, MD, MS, of Rochester, MN; Joy Moverley, DHSc, MPH, PA-C, of Vallejo, CA; Sean M. Oser, MD, MPH, of Aurora, CO; Alissa R. Segal, PharmD, CDCES, CDTC, FCCP, of Boston, MA; and Jennifer Trujillo, PharmD, FCCP, BCPS, CDCES, BC-ADM, of Aurora, CO. Christopher W. Jones, MD, of Murray, UT; Scott J. Pilla, MD, MHS, of Baltimore, MD; and Nay Linn Aung, MD, BC-ADM, of Utica, NY, also contributed abridged chapters. ADA staff support was provided by Caitlin Krekel, MSPH, RD, Sarah Bradley, and Raveendhara R. Bannuru, MD, PhD, FAGE.
The complete Standards of Care in Diabetes—2023 was developed by the ADA’s Professional Practice Committee: Nuha Ali ElSayed, MD, MMSc (Chair), Grazia Aleppo, MD, Vanita R. Aroda, MD, Raveendhara R. Bannuru, MD, PhD, FAGE (Chief Methodologist), Florence M. Brown, MD, Dennis Bruemmer, MD, PhD, Billy S. Collins, DHSc, PA-C, Marisa E. Hilliard, PhD, Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCP, Eric L. Johnson, MD, Scott Kahan, MD, MPH, Kamlesh Khunti, MD, PhD, FRCP, FRCGP, FMedSci, Jose Leon, MD, MPH, Sarah K. Lyons, MD, Mary Lou Perry, MS, RDN, CDCES, Priya Prahalad, MD, PhD, Richard E. Pratley, MD, Jane Jeffrie Seley, DNP, MPH, MSN, BSN, RN, GNP, BC-ADM, CDCES, CDTC, FADCES, FAAN, Robert C. Stanton, MD, and Robert A. Gabbay, MD, PhD. American College of Cardiology—Designated Representatives (Section 10) include Sandeep R. Das, MD, MPH, FACC, and Mikhail Kosiborod, MD, FACC, FAHA. Designated subject matter experts are Kenneth Cusi, MD, FACP, FACE, Christopher H. Gibbons, MD, MMSc, John M. Giurini, DPM, Lisa Murdock, Jennifer K. Sun, MD, MPH, Crystal C. Woodward, Deborah Young-Hyman, PhD, FTOS, and Fel SBM, CDCES. ADA staff are Raveendhara R. Bannuru, MD, PhD, FAGE, Nuha Ali ElSayed, MD, MMSc, Robert A. Gabbay, MD, PhD, Malaika I. Hill, MA, and Laura S. Mitchell.